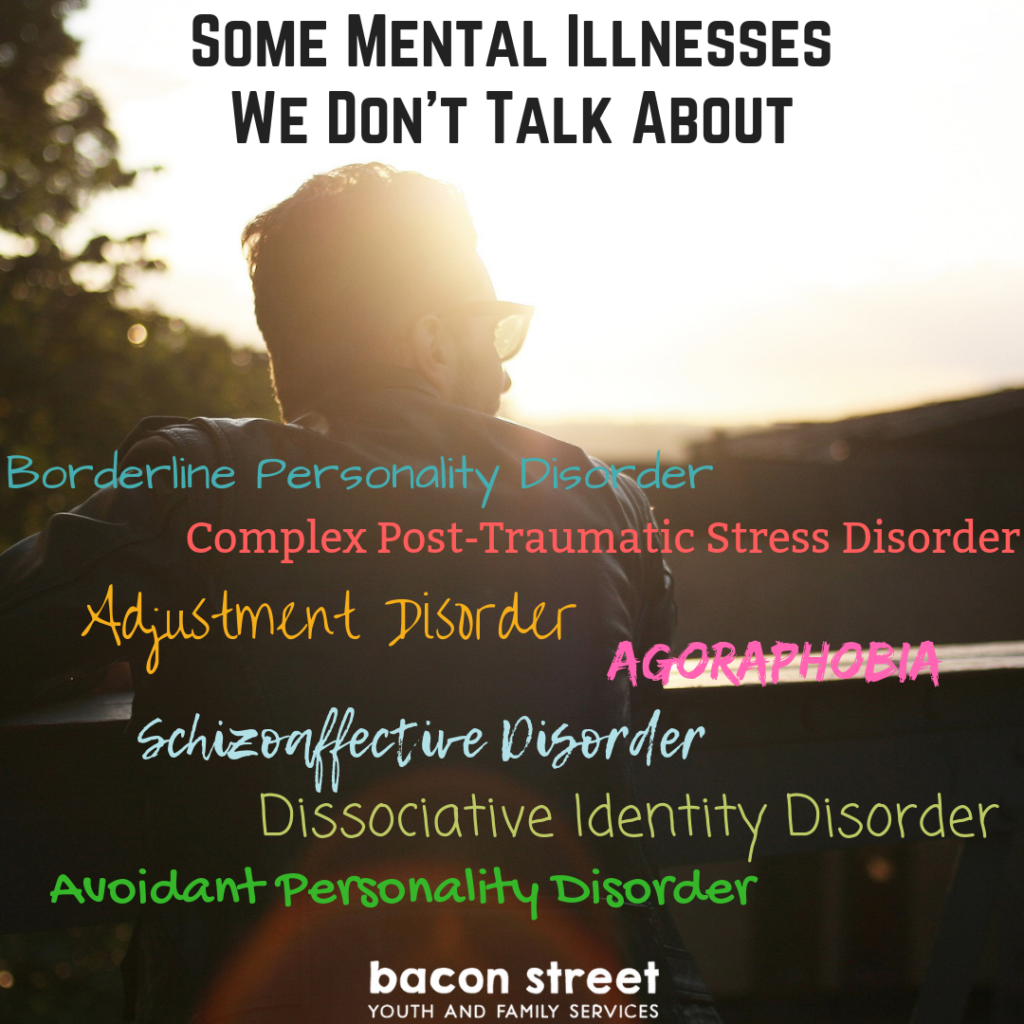
It’s Mental Illness Awareness Week! With over 200 classified forms of mental illness, it seems like we mostly focus on depression, anxiety, and bipolar disorder. Since this week is all about raising awareness, I thought we could talk about a few that you may have heard about but are highly stigmatized, and some that you may not have heard about at all.
This list comes from a great article on The Mighty called 15 Types of Mental Illnesses We Don’t Talk About. While I didn’t discuss each one (phew, that would have been a long blog post) I did want to talk a little bit more some of these, so we can destigmatize these mental illnesses and raise awareness. I also recommend you check out the original article. Each illness has links to personal stories of those who have the disease.
- Borderline Personality Disorder
Those who have Borderline Personality Disorder, or BPD, are unable to manage emotions effectively. Sometimes it affects all relationships, sometimes only one. Some people are high functioning in certain settings while their personal lives may be in turmoil. And BPD usually begins during adolescence or early adulthood.
Some of the major symptoms include an ongoing pattern of varying moods, self-image, and behavior, which result in impulsive actions and the difficulty with relationships mentioned above. Other symptoms include self-harming, suicidal thoughts, feelings of emptiness, difficulty with trust, feelings of dissociation, and more. Not everyone will suffer all of the symptoms, as some have only reported having some of the symptoms of this illness.
- BPD affects 5.9% of adults (about 14 million Americans) at some time in their life.
- BPD affects 50% more people than Alzheimer’s disease and nearly as many as schizophrenia and bipolar combined (2.25%).
- BPD affects 20% of patients admitted to psychiatric hospitals.
- BPD affects 10% of people in outpatient mental health treatment.
Research on the causes of BPD is still ongoing, but scientists do agree that genetic and environmental influences are likely to be involved. Harmful childhood experiences, such as emotional, physical, and sexual abuse as well as loss, neglect, and bullying can further increase the risk. BPD is treatable and many individuals find a decrease in their impulsive behavior in their 40’s.
One of the issues that cause this mental illness to be stigmatized is the name. At one time, BPD used to be considered on the “borderline” between psychosis and neurosis. Even though it does not describe the condition very well, the name still stuck. Some consider “Emotion Disregulation” to be a better name and a better reflection of what the disease really is.
- Complex Post-Traumatic Stress Disorder (C-PTSD)
This one is still pretty new, and should not be confused with Post-Traumatic Stress Disorder, of PTSD. Complex Post-Traumatic Stress Disorder results from ongoing or repeated interpersonal trauma where the victim is traumatized in captivity and there is no perceived way to escape. Examples of captivity can include ongoing child abuse, domestic violence, and forced prostitution/sex trafficking. This isn’t from a one-time event, but a recurring event that changes the brain and the person’s worldview.
Survivors of C-PTSD report a deep fear of trust, terminal loneliness, problems with regulation emotions, flashbacks, hypervigilance, helplessness, shame, dissociation, suicidal thoughts, and more.
- Dissociative Identity Disorder (DID)
This disorder tends to be misunderstood due to media misrepresentation. Often times, the serial killer in a television show or movie will be said to have Dissociative Identity Disorder, or DID. And that is pretty much the only attention and exposure the disorder gets. However, this should be treated as a serious mental illness and not treated as Hollywood entertainment or a great storyline.
DID used to be referred to as multiple personality disorder up until 1994, although you still may hear some refer to it that way. The person’s identity is fragmented into two or more distinct personality states. The identities usually take turns controlling the individual. Memory loss is also part of this disorder and it goes beyond normal forgetfulness.
For someone to be diagnosed with this disorder, they must:
- Have two or more distinct personality states.
- The disruption in identity involves a change of self, sense of agency, and changes in behavior, consciousness, memory perception, cognition, and motor function.
- Frequent gaps are found in memories of personal history.
- These symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The cause of DID is not quite understood, but it does seem to appear more often in those who have experiences physical and sexual abuse, especially during their childhood. It can appear at any age and can be coupled with PTSD symptoms.
- Agoraphobia
That name might be a mouthful, but this one is pretty interesting to learn about. It is actually a type of anxiety disorder. People purposefully avoid certain places or situations that make them feel trapped, helpless, panicked, embarrassed, and/or scared. They may experience something like that of a panic attack. There are instances so severe that it can stop people from doing daily activities. What is interesting is that most people that have agoraphobia realize their fear is irrational, but they are unable to do anything about
People with agoraphobia are typically afraid to leave their home for an extended period of time, afraid to be alone in the social situation they have a fear of, afraid to lose control in a public place, afraid to be in places where they may feel unable to escape, detached or estranged from others, and anxious or agitated.
The panic attack symptoms are chest pain, a racing heart, shortness or breath, dizziness, trembling, choking, sweating, hot flashes, chills, nausea, diarrhea, numbness, and/or tingling sensations.
Agoraphobia can be caused by depression, other phobias, other anxiety disorders, a history of physical or sexual abuse, substance abuse problem, and a family history of agoraphobia. It is also more common in women than it is in men.
- Avoidant Personality Disorder
This disorder is extreme shyness and fear of rejection that make it extremely difficult for those who have it to interact with others socially and professionally.
Symptoms include being easily hurt by criticism or disapproval, no close friends, reluctance to become involved with people, avoidance of activities or occupations that involve contact with others, shyness in social situations out of fear or doing something wrong, exaggeration of potential difficulties, showing excessive restraint in intimate relationships, feeling socially inept, and unwilling to take risks or try new things because they may prove embarrassing.
Like many other mental illnesses, the cause is unknown but genetics and environmental factors appear to play a role in developing this condition.
- Schizoaffective Disorder
Schizoaffective Disorder is a chronic mental health condition with the symptoms of both schizophrenia and a mood disorder. Many may be diagnosed with either schizophrenia OR bipolar disorder since there are so many shared symptoms. But this disorder is rare and only seen in about 0.3% of the population.
People may experience different symptoms depending on what mood disorder is diagnosed, but here are some different symptoms:
- Hallucinations
- Delusions
- Disorganized thinking
- Depressed mood
- Manic behavior
Again, with this mental illness, the cause is unknown. It appears that there is a few things that work together to cause this disorder, such as genetics, brain chemistry, stress, and possibly drug use.
Diagnosing this disorder can be hard, but there are two types of schizoaffective disorder: bipolar type and depressive type. To be diagnosed with schizoaffective disorder, a person must have the following symptoms:
- A period during which there is a major mood disorder, either depression or mania, that occurs at the same time that symptoms of schizophrenia are present
- Delusions or hallucinations for two or more weeks in the absence of a major mood episode.
- Symptoms that meet criteria for a major mood episode are present for the majority of the total duration of the illness.
- The abuse of drugs or a medication is not responsible for the symptoms.
- Adjustment Disorder
Adjustment disorder, sometimes called Situational Depression, is an abnormal and excessive reaction to an identifiable life stressor. This can be from a single life event, or multiple events. They can also be recurrent events or continuous. Symptoms must arise within three months of the onset of the stressor and last no longer than six months after the stressor has ended. It is also associated with a high risk of suicide or suicidal behavior, substance abuse, and the prolongation of other medical disorders or interference with their treatment.
Symptoms include depressed mood, impaired occupational/social functioning, agitations, trembling or twitching, physical complaints, palpitations, conduct disturbances, withdrawal, anxiety, worry, stress, and tension. But symptoms can vary greatly, and the person may not even realize what the stressor was that caused the disturbance.
Diagnosis depends on the following:
- The reaction clearly follows a life stressor. Within three months of stressor onset, emotional and behavioral symptoms develop in response to stressor.
- Symptoms seem excessive compared to what would normally be expected in relation to stressor and/or symptoms significantly impair occupational, school, or social functioning.
- Symptoms are not explained by another diagnosis.
- Symptoms are not part of bereavement.
- Symptoms do not last longer than six months after end of stressor.
- The diagnosis may be acute (symptoms last less than six months) or chronic (symptoms last six months or longer as when stressors are chronic or have lasting effects).
Sources:
- https://themighty.com/2018/06/uncommon-unknown-mental-illnesses/
- https://www.nimh.nih.gov/health/topics/borderline-personality-disorder/index.shtml
- https://themighty.com/2017/08/life-impacting-symptoms-of-complex-post-traumatic-stress-disorder-ptsd/
- https://www.psychologytoday.com/us/conditions/dissociative-identity-disorder-multiple-personality-disorder
- https://www.healthline.com/health/agoraphobia#outlook
- https://www.psychologytoday.com/us/conditions/avoidant-personality-disorder
- https://www.nami.org/Learn-More/Mental-Health-Conditions/Schizoaffective-Disorder
- https://www.psychologytoday.com/us/conditions/adjustment-disorder