It is important to discuss and address both mental health and addiction together, because having a mental illness makes it more common to also suffer from a substance use disorder at the same time, or vice versa. This week on the blog, we are discussing the ins and outs of dual diagnosis, or co-occurring disorders.
What is a dual diagnosis? Also known as a co-occurring disorder, this is a term used for someone who experiences a mental illness and a substance use disorder simultaneously. Either one can occur first. Those experiencing a mental illness may turn to alcohol and/or drugs to cope and self-medicate. Although, it has been found that substances such as alcohol and drugs actually worsen their mental illness symptoms.
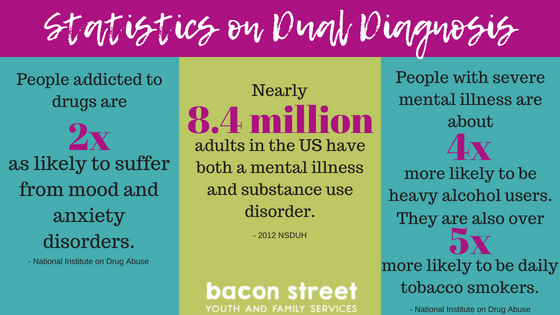
Is it common? Yes! In 2014, the National Survey on Drug use and Health showed that 7.9 million people in the United States experience both a mental illness and substance use disorder simultaneously. More than half (4.1 million) are men. According to dualdiagnosis.org, up to 65.5% of people with a substance use disorder had at least one mental disorder and 51% of people with a mental disorder had at least one substance use disorder.
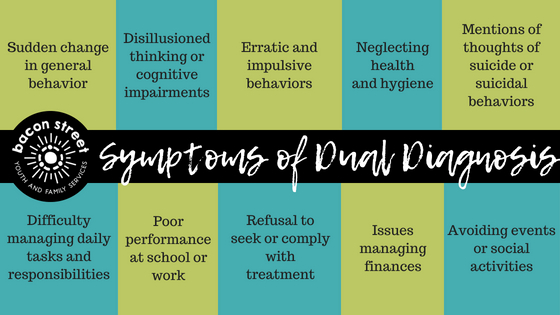
What are the symptoms? This is where it gets tricky. Because there are many combinations that can occur, symptoms vary greatly. You have to know the symptoms of the substance being usd and the symptoms of the mental health condition. You can see the overlap of the symptoms below.
A few symptoms of substance use disorder can include:
- Withdrawal from friends and family
- Sudden changes in behavior
- Using substances under dangerous conditions
- Engaging in risky behaviors
- Loss of control over use of substances
- Developing a high tolerance
- Feeling like you need a drug to be able to function
A few symptoms of a mental illness can include:
- Extreme mood changes
- Confused thinking
- Problems concentrating
- Avoiding friends, family, and/or social activities
- Thoughts of suicide
What are some common mental health issues that occur with addiction? According to addictioncenter.com, there are a few mental health/behavioral issues that repeatedly occur alongside addiction. Sometimes, they are even the underlying cause of addiction, so you should pay attention to the symptoms when determining a long-term recovery plan.
- Attention-deficit hyperactive disorder (ADHD): People with ADHD may be more inclined to abuse substances to cope with their symptoms. The stimulants they are prescribed for ADHD can also be habit-forming and lead to a toxic pattern of substance use.
- Bipolar Disorder: About half of people with bipolar disorder also struggle with addiction. They self-medicate with drugs and/or alcohol as temporary relief from emotional situations and manic episodes.
- Borderline Personality Disorder: Over two-thirds of people with Borderline Personality Disorder have also suffered from substance abuse at some point in their lives.
- Depression: 1 in 10 adults in the United States have reported suffering from depression. Drugs and/or alcohol are used to self-medicate, which can actually make the problem worse. The crash that occurs after the high can be devastating to those with depression.
- Eating Disorders: Drugs that suppress the appetite are commonly used among people with eating disorders.
- Generalized Anxiety Disorder (GAD): This is the most common mental health condition in the United States. It affects 18% of adults. Again, drugs and/or alcohol are used to self-medicate. Benzodiazepines may also be abused, as they are a highly addictive prescription medication used to treat anxiety disorders.
- Obsessive Compulsive Disorder (OCD): With OCD sometimes comes anxiety and depression due to their involuntary behavior. As mentioned above, both of these can lead to substance use.
- Post-traumatic Stress Disorder (PTSD): When someone has PTSD, their brain produces less endorphins than a healthy brain would. This makes them more likely to turn toward drugs and/or alcohol to feel happiness.
- Schizophrenia: Diagnosing schizophrenia alongside an addiction can be difficult due to the fact that both conditions can have the same effects on a person. With schizophrenia, as with other mental illnesses, drugs and/or alcohol are used to self-medicate.
Overlapping factors that can aggravate a mental health or substance abuse disorder:
- Brain responses: Drug abuse can cause symptoms that mimic a mental illness. Marijuana can cause psychosis. Many drugs can cause hallucinations and paranoia.
- Genetics: Genes make up 40 – 60% of a person’s susceptibility to addiction.
- Environmental triggers: Stress, anxiety, or a traumatic event can start an addiction or mental disorder.
- Exposure at a young age: Experimenting with drugs and/or alcohol at a young age while the brain is developing can cause damage. Also, substance use at a young age makes it likely that they will develop a problem later on in adulthood.
How is it treated? Both problems must be addressed for a successful outcome! It is important to work with a professional on how one condition affects the other to come up with an effective and successful treatment plan. This may differ from person to person, but below are some common methods that may be part of that plan.
- Detoxification: Inpatient detox is found to be more effective than outpatient detox, but this is the first major hurdle they will face. Inpatient detox involves medical staff monitoring 24/7 for up to seven days. This may involve administering tapering amounts of the substance (or its medical alternative) to wean the person off and lessen the effects of withdrawal.
- Inpatient Rehabilitation: Treatment centers that provide both medical and mental health care 24/7 can be extremely beneficial for someone experiencing a dual diagnosis. Therapy, support, medication, and health services are used to treat both the substance use disorder and mental illness at the same time.
- Supportive Housing: Residential treatment centers, such as group homes or sober living homes, are a great transition into society after detox and rehab. These centers are crucial in providing support and independence while trying to avoid relapse when newly sober. However, be careful about which center you choose. Not all centers are run by licensed professionals, which has left the quality of care in question. Do your research and pick a reputable center.
- Psychotherapy: This is a large part of effective dual diagnosis treatment, especially CBT (cognitive behavioral therapy). This particular therapy helps people cope and change ineffective patterns of thinking to reduce the chances of substance use.
- Medications: This is very important, especially in treating mental illnesses. Some medications can also help with substance use disorder withdrawal symptoms, especially during the detox phase.
- Self-help and Support Groups: Reaching out and finding those who have experienced dual diagnosis as well can help with feelings of loneliness and isolation. They provide hope and an outlet to voice frustrations, as well as share their story. Double Trouble in Recovery, Alcoholics Anonymous, Narcotics Anonymous, and Smart Recovery are just a few of the groups out there. See what groups are in your community and join.
Sources:
https://www.nami.org/Learn-More/Mental-Health-Conditions/Related-Conditions/Dual-Diagnosis